How the Gut Microbiome interacts with The mucus layer
Let me introduce you to the Mucus Layer
Both the skin and the mucus layer are barriers that cover anatomical surfaces. The mucus layer is found covering the eyes and organs of the respiratory, gastrointestinal, and reproductive tracts. The main function is to physically prevent the microbiota and other substances from contacting the epithelial cells.
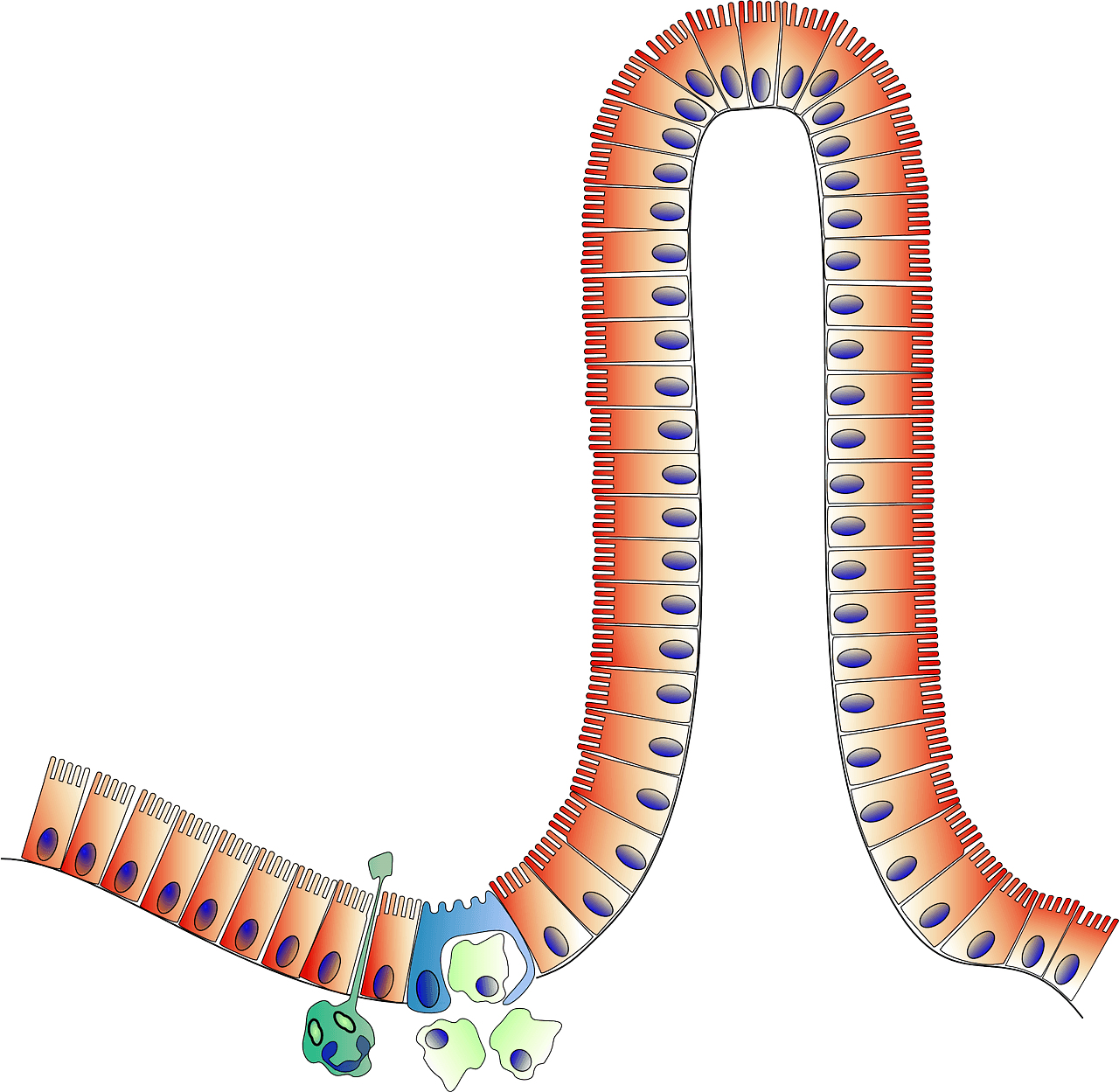
Depending on the location, the mucus layer is more or less thick and compact. For instance, in the colon, the mucus layer is divided into 2 layers: an outer loose layer where the bacteria stay, and an inner dense layer that excludes microbiota. On the contrary, the mucus layer of the small intestine is thinner, loosely attached to the epithelial cells, and is easily penetrable by bacteria and nutrients.
Surprisingly, the mucus layer is much more than a physical barrier. It also binds and retains molecules of the immune system, including immunoglobulin A (IgA), metabolites, antimicrobial peptides (defensins), and other molecules with protective capacity (such as lysozyme).1 But this is not all! The mucus layer participates in many other cellular functions such as cell growth, differentiation, signaling, tight junction regulation, and tumor progression.2
What can happen if the thickness of the mucus layer is altered?
This is a common feature of inflammatory bowel diseases (IBDs), including Ulcerative colitis (UC) and Crohn’s disease (CD), both of which increase the risk of colorectal cancer.3, 4, 5
Meet Mucins, huge proteins that form the mucus layer
The mucus layer gets its name from being a gel-like structure formed by large proteins called mucins. These proteins are glycoproteins, which means that are covered by carbohydrates (also called O-glycans) accounting for more than 50% of their mass. Because these O-glycans bind to water, the mucus layer obtains the consistency of a gel/mucus.1
Mucins can be divided into two groups: transmembrane mucins (attached to the surface of epithelial cells) and soluble mucins (which form the outer mucus layer).6 Epithelial cells produce transmembrane mucins that get attached to their membrane, while soluble mucins are only produced by specialized cells called goblet cells.
Microbiome and the Mucus layer: a symbiotic relationship
You may have heard that we are 10 times more bacterial cells than human cells! This is outdated. I wrote a blog post about it too. The ratio of microbial to human cells is closer to 1,3:1, and most of these bacteria are found in the colon.
How do our colon epithelial cells deal with such huge amounts of bacteria?
Thanks to the mucus layer, the colon epithelial cells are separated from the microbiota. Bacteria are found in the outer mucus layer since it is less compact. We could say that this is the natural habitat of our intestinal microbiota.
There are a few reasons why a mucus layer is an ideal place for our microbiota. This region is especially important for bacteria that feed on carbohydrates because mucins are 50% carbohydrates! Bacteria have specialized proteins (adhesins) that bind to different glycans (carbohydrate structures) on mucins, as well as enzymes that cleave and transport these glycans into the bacteria to be used as energy. In this way, bacteria prevent being flushed away by the intestinal fluids and are in an environment rich in food.
For our cells, this is a favorable situation too! Usually, bacteria that live in the outer mucus layer are less virulent and do not form biofilms on top of the epithelial cells, and limit the amount of space for pathogenic bacteria. To maintain this symbiotic relationship, our cells must constantly produce mucins. It is thought that one of the beneficial effects of probiotic bacteria is to enhance mucin production and strengthen the intestinal cell monolayer through tight junction regulation.1
Have you wondered why we have different microbiota depending on the anatomical location we look at?
One reason is that the glycan structures that cover mucins differ. Because bacteria bind to these carbohydrates in a very specific manner, there is a selection for specific microbiota in each anatomical region. This interaction is so important that some pathogenic bacteria, such as Helicobacter pylori, induce changes in the carbohydrate composition according to their needs.1
When the symbiotic relationship gets broken…
Some bacteria break this relationship and start taking more than our cells can handle.
It can be the case that they grow into big populations very quickly, there is a breach in the mucus layer, or simply it was their first intention. In fact, some bacteria are almost always pathogenic while others become pathogenic just because they can in certain situations.
Very motile bacteria that secrete mucin-degrading enzymes and establish beneficial relationships with other bacteria, can end up compromising the integrity of the mucin layer. After reaching the surface of epithelial cells, some bacteria can release toxins that compromise the integrity of the epithelial cells. For example, by disrupting the proteins (called tight junctions) that connect epithelial cells.1
As a way to combat some of these situations, transmembrane mucins can also be automatically cleaved and released to the lumen in response to certain bacteria attaching to them.
Moreover, part of these transmembrane mucins is found inside the cells (cytoplasmic tail) and can activate pathways inside the cells that lead to changes in response to bacteria.
In some cases, mucins can have direct antimicrobial activity. Certain mucin carbohydrates can inhibit the growth of specific bacteria, an effect that has already been shown for Helicobacter pylori.7
Another strategy commonly used by pathogenic bacteria is to avoid the mucus layer by binding to M cells. These cells are specifically designed to capture bacteria and show them to immune system cells found in the underlying tissue. In this region of the epithelial barrier, there are fewer goblet cells, thus the mucus layer is much thinner. Despite M cells being only a small percentage of all mucosal epithelial cells, some microbes can use them as a direct entry into the deeper tissue.7

What can you do to maintain a healthy mucus layer?
Eat a fiber-rich diet, aka plants!
Bacteria eat what we eat. However, most beneficial bacteria prefer to eat what is left after we digest plants, fiber! The composition of the food you eat is thus the number one factor that changes microbiota, from day to day, from meal to meal. A fiber-limited diet such as the carnivore and Western diets will promote the expansion of bacteria that feed on the mucus layer. You can imagine that if this relationship gets uncontrolled, for example by an overgrowth of mucin-degrading bacteria, the mucus layer will be compromised.1
Apply the necessary lifestyle measures to reduce chronic inflammation: increase physical activity, eat a healthy diet, reduce exposure to environmental and industrial toxins, and lower your psychological stress.8